Understanding and Managing Gut Health and Dysbiosis
Our bodies host trillions of bacteria, with the largest colonies residing in our digestive system. Beneficial bacteria play a crucial role in maintaining health by helping us digest nutrients and keeping potentially harmful bacteria in check. However, a modern diet and lifestyle can disrupt this balance, leading to conditions such as constipation, IBS, and a weakened immune system.
What is Dysbiosis?
Dysbiosis refers to an imbalance of microbes in the digestive tract. Unlike immediate infections like salmonella, dysbiosis often involves low-virulence microbes that cause ongoing inflammation and health problems. Common symptoms include:
- Inflammation
- Pain
- Swelling
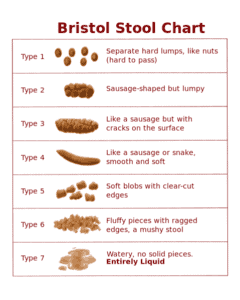
- Digestive issues
These symptoms are often masked by medications, which can further suppress the body’s natural healing responses.
Causes of Dysbiosis
Several factors contribute to dysbiosis:
- Ongoing stress
- Chemical exposure
- High-sugar and processed food diets
- Chronic use of medications (e.g., oral contraceptives, antibiotics, steroids, NSAIDs)
- Low-fiber diets (which slow down digestion and promote bacterial growth)
- Reduced digestive enzyme output (common in Type 2 Diabetes)
- Reduced stomach acid (from long-term use of proton pump inhibitors)
Common Forms of Dysbiosis
- Candida Overgrowth: Candida albicans is a yeast naturally present in the gut. When it overgrows, it can cause symptoms like anxiety, abdominal bloating, fatigue, and strong sugar cravings.
- Helicobacter pylori: This bacterium is a common cause of stomach ulcers and poor digestion.
- Small Intestinal Bacterial Overgrowth (SIBO) and Intestinal Methanogen Overgrowth (IMO): These conditions can lead to irritable bowel syndrome (IBS).
Managing Dysbiosis
Dietary Changes:
- Avoid feeding harmful microbes by cutting out sugar, alcohol, yeast, vinegar, and high-carb foods.
- Focus on a high-fiber diet with plenty of vegetables, proteins, healthy fats, nuts, seeds, and whole fruits.
- Consider adding supplemental fiber, such as ground psyllium husks or flaxseeds.
- Avoid feeding harmful microbes by cutting out sugar, alcohol, yeast, vinegar, and high-carb foods.
Natural Remedies:
- For Candida: Garlic, undecylenic acid, grapefruit seed extract, capryllic acid, oregano oil, berberine, and pau d’arco extract.
- For H. pylori: Mastic gum.
- General Gut Healing: Glutamine, aloe vera, deglycyrrhizinated licorice (DGL), slippery elm, marshmallow root, cabbage juice, and zinc carnosine.
- For Candida: Garlic, undecylenic acid, grapefruit seed extract, capryllic acid, oregano oil, berberine, and pau d’arco extract.
Probiotics:
- Support healthy bacteria by taking a daily probiotic supplement or eating cultured, fermented foods. Start with a small amount and gradually increase to a significant daily dose (e.g., at least 15 billion CFUs of a multi-strain probiotic).
- Support healthy bacteria by taking a daily probiotic supplement or eating cultured, fermented foods. Start with a small amount and gradually increase to a significant daily dose (e.g., at least 15 billion CFUs of a multi-strain probiotic).
Managing Die-Off Reactions:
- When harmful bacteria die, they can release toxins that temporarily worsen symptoms. Activated charcoal can help manage these reactions.
- When harmful bacteria die, they can release toxins that temporarily worsen symptoms. Activated charcoal can help manage these reactions.
Final Note
Rebalancing your gut flora takes time. Implement dietary changes and natural remedies consistently for at least three months, then reintroduce other foods slowly, monitoring your symptoms.
If you would like some customized support to delve deeper into your health and nutrition, let’s chat.
Resources: Lipski, Elizabeth, Digestive Wellness, McGraw-Hill, 2005 and Hyman, Dr. Mark, Ultraprevention, Atria, 2005. © Purpose Inc., The School of Applied Functional MedicineTM